Assisted reproductive technology (ART) refers to a group of medical treatments and procedures used to help people conceive a child when they are experiencing fertility problems. ART involves using advanced reproductive technologies to assist with fertilization, embryo development, and implantation of embryos in the uterus. Assisted Reproductive Technology (ART) refers to several variations in treatment tailored to patients' unique conditions. These procedures are usually paired with more conventional therapies, such as fertility drugs, to increase success rates. ART has helped many people to conceive a child who may not have been able to do so without medical assistance.
The main ART techniques
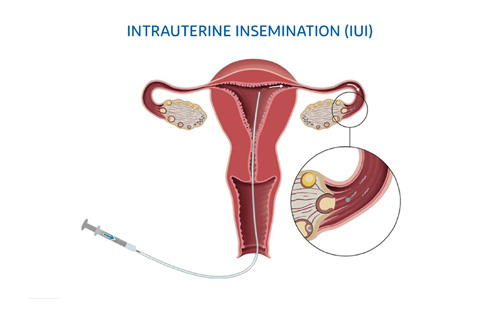
Intrauterine Insemination (IUI):
IUI stands for intrauterine insemination, which is a fertility treatment where sperm is inserted directly into the uterus through a small catheter. IUI is typically used for couples who are experiencing infertility due to issues such as low sperm count, endometriosis, or cervical factors, or for individuals or couples who are using donor sperm.
The process of IUI typically involves monitoring ovulation using ultrasound and blood tests to determine the optimal time for insemination. Sperm is collected, washed, and concentrated in a laboratory, and then inserted directly into the uterus using a small catheter.
IUI is a less invasive and less expensive option compared to other fertility treatments such as in vitro fertilization (IVF). It can be done with or without fertility medications to stimulate ovulation, depending on the individual or couple's specific situation.
This procedure is combined with hormone treatments to boost egg production can help couples with low sperm count, unexplained infertility, or cervical mucus problems. Semen is collected, and then delivered via a catheter inserted through the women's vagina and cervix to her uterus. The success rate of IUI varies depending on a number of factors, including the age of the individuals, the underlying cause of infertility, and the use of fertility medications.
In vitro fertilization (IVF):
IVF stands for in vitro fertilization, which is a fertility treatment that involves combining sperm and eggs outside of the body in a laboratory. The resulting embryos are then transferred into the uterus with the goal of achieving a successful pregnancy.
The process of IVF typically involves several steps. First, a woman undergoes a course of fertility medications to stimulate the ovaries to produce multiple eggs. Then, eggs are retrieved from the ovaries using a minimally invasive procedure called transvaginal ultrasound-guided follicle aspiration. The retrieved eggs are then fertilized in a laboratory with sperm, and the resulting embryos are cultured for several days.
After the embryos have been cultured, one or more embryos are transferred into the uterus using a catheter. Any remaining embryos may be frozen for future use. A pregnancy test is performed approximately two weeks after the embryo transfer to determine if the IVF cycle was successful.
IVF can be an effective treatment for a range of fertility issues, including male factor infertility, tubal factor infertility, endometriosis, and unexplained infertility. It can also be used in cases where other fertility treatments, such as IUI, have not been successful. The success rate of IVF also varies depending on a number of factors, including the age of the individuals, the underlying cause of infertility, and the quality of the embryos.
Overall, IVF can be a useful option for individuals and couples who are experiencing infertility and have not been successful with other treatments. However, it is important to discuss the benefits and limitations of IVF with genome consultant to determine if it is the most appropriate treatment option for each individual or couple.
Intracytoplasmic sperm injection (ICSI):
ICSI stands for intracytoplasmic sperm injection, which is a type of assisted reproductive technology (ART) used in cases of male factor infertility. ICSI involves the injection of a single sperm directly into an egg in order to facilitate fertilization and improve the chances of a successful pregnancy.
ICSI is typically used in cases where the male partner has a low sperm count, poor sperm motility, or other sperm-related issues that make fertilization difficult. The process of ICSI is similar to that of IVF, in which fertility medications are used to stimulate the ovaries to produce multiple eggs, which are then retrieved from the ovaries using a minimally invasive procedure.
After the eggs are retrieved, they are held in place using a specialized pipette, while a single sperm is injected directly into the egg using a very fine needle. After the injection, the fertilized egg (embryo) is cultured for several days before being transferred to the uterus using a catheter.
ICSI can improve the chances of a successful pregnancy in cases of male factor infertility, and it may also be used in cases where previous attempts at IVF have not been successful. It is important to discuss the benefits and limitations of ICSI with our genome consultant to determine if it is the most appropriate treatment option for each individual or couple.
Preimplantation genetic diagnosis (PGD):
PGD stands for preimplantation genetic diagnosis, which is a reproductive technology used during in vitro fertilization (IVF) to test embryos for genetic disorders before they are transferred to the uterus. PGD is typically used when one or both partners have a known genetic disorder, or when they are at risk of passing on a genetic disorder to their offspring.
The process of PGD involves the removal of one or more cells from an embryo during the early stages of development. The cells are then tested for specific genetic abnormalities using specialized laboratory techniques, such as polymerase chain reaction (PCR) or fluorescence in situ hybridization (FISH).
Embryos that test negative for the genetic disorder can then be transferred to the uterus for implantation. This can help to reduce the risk of passing on a genetic disorder to future generations.
PGD can be used to test for a wide range of genetic disorders, including cystic fibrosis, sickle cell anemia, and Huntington's disease, among others. It may also be used in cases where the parents are carriers of a genetic disorder but do not show any symptoms themselves.
It is important to discuss the benefits and limitations of PGD with our genome consultant and genetic counsellor to determine if it is the most appropriate treatment option for each individual or couple.
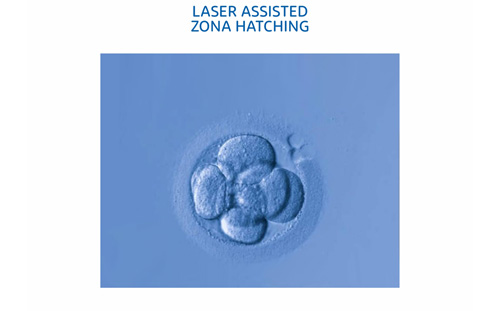
Assisted Hatching:
Assisted hatching is a technique used during in vitro fertilization (IVF) to help embryos hatch out of their protective outer layer (zona pellucida) and implant into the lining of the uterus. The technique involves making a small hole or thinning a section of the zona pellucida using a laser or chemical treatment.
Assisted hatching is typically used in cases where the zona pellucida of the embryo is abnormally thick or hard, which can make it more difficult for the embryo to hatch and implant. It may also be used in cases where the woman is older or has had previous unsuccessful IVF cycles.
The procedure of assisted hatching is performed shortly before the embryo transfer, after the embryos have been cultured in the laboratory for several days. The procedure is typically performed on only a select number of embryos, as not all embryos are suitable for assisted hatching.
It is important to discuss the benefits and risks of assisted hatching with genome consultant and embryologists to determine if it is the most appropriate treatment option for each individual or couple.
Donor Sperm:
Donor sperm is often used in fertility treatments when a male partner's sperm is not available or when there is a risk of genetic disease. Fertility clinics usually have their own sperm banks, which carefully screen and select sperm donors based on various criteria, such as age, medical history, and genetic testing. The use of donor sperm can be a viable option for couples or individuals who are experiencing fertility issues. The process typically involves the fertilization of an egg using donor sperm, either through intrauterine insemination (IUI) or in vitro fertilization (IVF).
Donor Egg:
Donor egg is a reproductive technology used in cases where a woman's own eggs are not viable or of poor quality, or if there is a risk of passing on a genetic disorder to the offspring. In donor egg treatment, eggs from a donor are used instead of the woman's own eggs for fertilization with sperm, typically via in vitro fertilization (IVF).
The process of donor egg treatment typically involves selecting a donor who is typically younger, healthy and has undergone screening tests for infectious diseases and genetic disorders. The donor's eggs are then retrieved from her ovaries using a minimally invasive procedure, and fertilized with the sperm of the intended father or a donor sperm. The resulting embryos are then cultured in a laboratory for several days, after which one or more embryos may be transferred to the uterus of the intended mother or a surrogate.
Donor egg treatment can be an effective option for women who are unable to conceive with their own eggs due to various reasons including advanced maternal age, premature ovarian failure, or genetic disorders. It can also be used in cases where previous attempts at IVF with the woman's own eggs have been unsuccessful. Donor egg treatment typically has higher success rates compared to IVF with the woman's own eggs, especially in women over the age of 40.
It is important to discuss the benefits and limitations of donor egg treatment with Genome consultant to determine if it is the most appropriate treatment option for each individual or couple.
Surrogacy or use of a gestational carrier:
Another woman carries your embryo, or a donor embryo, to term and gives the baby to you after birth. Surrogacy can be a viable option for individuals or couples who are unable to carry a pregnancy to term due to medical conditions or other factors. It can also be an option for same-sex male couples who wish to have biological children. However, surrogacy can raise emotional, legal, and ethical issues, and the laws surrounding surrogacy vary widely depending on the country and state. It is important to consult with the fertility centre before pursuing surrogacy.
** Surrogacy/Gestational Carrier Services at presently is not done at Genome - The Fertility Centre.
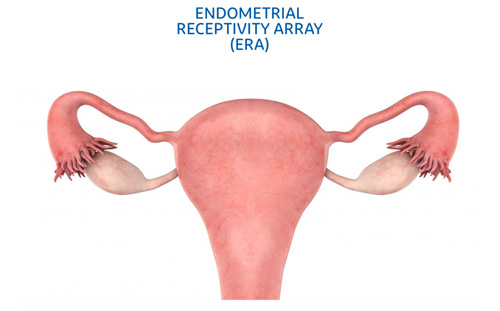
ERA:
Endometrial receptivity analysis (ERA) is a diagnostic test that is used in infertility treatment to determine the optimal time for embryo transfer in in vitro fertilization (IVF) cycles. Endometrial Receptivity Array (ERA), a relatively new procedure that helps determine whether it is the optimal time for an embryo to be transferred into a uterus for embryo implantation. Problems in endometrial lining are can cause infertility in women with recurrent pregnancy loss or multiple failure in IVF. ERA procedure is done to predict the ideal implantation window for the patients with such problems.
Fertility Preservation:
Fertility preservation is the method of preserving eggs and sperm so that the couple can use them to have biological children in future. Couples with certain diseases and disorders that affect fertility or those wanting to postpone pregnancy may benefit from fertility preservation. At Genome we have well equipped cryology laboratory for storing the eggs and sperm for such later use.
FET:
A frozen embryo transfer (FET) cycle is a process that uses embryos that have been frozen During the FET cycle, the embryos are thawed and placed into the uterus. This is done at a time in your menstrual cycle that best supports a pregnancy. Frozen Embryo Transfer (FET) is a type of Fertility Enhancement Technology (FET) that involves thawing and transferring previously frozen embryos into the uterus of a woman who is trying to conceive. The embryos are typically frozen after being created through in vitro fertilization (IVF), allowing for their storage until they are needed. FET can be a useful option for individuals or couples who have undergone IVF but did not use all of the embryos created during the process. By freezing and storing the excess embryos, they can be thawed and used in a future attempt at pregnancy, often with a higher success rate than a fresh embryo transfer. The process of FET typically involves taking medications to prepare the uterus for implantation and then transferring the thawed embryos into the uterus at the optimal time. The success rates of FET can vary depending on factors such as the age of the woman, the quality of the embryos, and any underlying fertility issues.
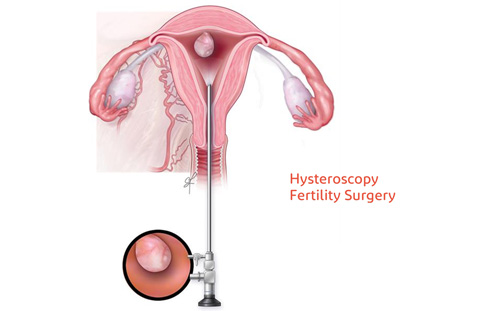
Hysteroscopy Fertility Surgery:
Hysteroscopy is a minimally invasive surgical procedure that can be used to diagnose and treat certain fertility issues. During a hysteroscopy, a thin, lighted tube called a hysteroscope is inserted through the cervix and into the uterus, allowing the surgeon to view the inside of the uterus and identify any abnormalities. During a hysteroscopy, any identified issues can often be treated using specialized instruments inserted through the hysteroscope. For example, fibroids or polyps may be removed, scar tissue may be cut or burned away, and abnormalities in the shape or size of the uterus may be corrected.
Overall, hysteroscopy can be a useful tool in the diagnosis and treatment of certain fertility issues, helping to improve the chances of a successful pregnancy.
Laparoscopic Fertility Surgery:
Laparoscopic fertility surgery is a minimally invasive surgical procedure that can be used to diagnose and treat certain fertility issues that cannot be addressed through other means. During a laparoscopic procedure, a small incision is made near the navel and a thin, lighted tube called a laparoscope is inserted into the abdomen. The laparoscope allows the surgeon to view the reproductive organs and surrounding structures and perform any necessary surgical procedures.
Laparoscopic fertility surgery can be used to diagnose and treat a variety of fertility issues, including:
- Endometriosis: A condition in which the tissue that normally lines the inside of the uterus grows outside of it, causing pain and potentially affecting fertility.
- Ovarian cysts or tumors: These can interfere with ovulation and fertility.
- Blocked or damaged fallopian tubes: These can prevent the egg and sperm from meeting, resulting in infertility.
- Uterine abnormalities: These can interfere with implantation or cause pregnancy complications.
During laparoscopic surgery, the surgeon may be able to remove or correct any identified issues, such as endometriosis lesions or ovarian cysts. In cases where the fallopian tubes are blocked or damaged, the surgeon may be able to perform a tubal ligation reversal or open up the tubes using a technique called a salpingostomy. Overall, laparoscopic fertility surgery can be a useful tool in the diagnosis and treatment of certain fertility issues, helping to improve the chances of a successful pregnancy.
Blastocyst Culture:
Blastocyst culture is a laboratory technique used during in vitro fertilization (IVF) to allow embryos to develop to a later stage before they are transferred into the uterus. During traditional IVF, embryos are typically transferred into the uterus 2-3 days after fertilization, when they have developed into 4-8 cell embryos. In contrast, blastocyst culture involves allowing embryos to develop for an additional 2-3 days, until they reach the blastocyst stage.
The blastocyst stage is characterized by the formation of an inner cell mass, which will eventually become the fetus, and an outer layer of cells, which will become the placenta. By allowing embryos to develop to this stage in the laboratory, embryologists can more accurately select the most viable embryos for transfer, potentially improving the chances of a successful pregnancy.
During blastocyst culture, embryos are placed in a special culture medium that provides the necessary nutrients for growth and development. Embryologists monitor the embryos closely during this time, looking for signs of proper development and selecting the most viable embryos for transfer.
Overall, blastocyst culture can be a useful tool in the field of reproductive medicine, allowing for improved selection of embryos for transfer and potentially improving the chances of a successful pregnancy. However, not all embryos will develop to the blastocyst stage, and the success rates of blastocyst transfer can vary depending on a variety of factors, including the age and health of the individuals involved.
Fertility Consultation:
A fertility consultation is an appointment with reproductive specialist, to discuss issues related to fertility and reproductive health. During a fertility consultation, the consultant will typically review the medical history of the individual or couple and perform a physical exam to assess fertility potential. The consultation may also include testing, such as blood work, ultrasound, or semen analysis, to assess fertility status and identify any underlying issues that may be affecting fertility. Based on the results of these tests, the fertility specialist may make recommendations for treatment, such as medication to stimulate ovulation, intrauterine insemination (IUI), or in vitro fertilization (IVF).
In addition to medical testing and treatment options, a fertility consultation may also include discussion of lifestyle factors that can impact fertility, such as diet, exercise, and stress management. The medical professional may also provide information on alternative options for building a family, such as adoption or surrogacy. Overall, a fertility consultation can be a valuable tool for individuals or couples who are experiencing difficulty conceiving or who have concerns about their reproductive health. By working with a genome fertility specialist consultant, the couple can receive a comprehensive evaluation of their fertility potential and receive guidance on the best options for achieving their reproductive goals.
TESA:
TESA stands for Testicular Sperm Aspiration, which is a procedure used to collect sperm directly from the testicles of men who have obstructive or non-obstructive azoospermia, a condition where there is no sperm in the semen. The collected sperm can then be used for in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI).
The TESA procedure involves inserting a fine needle into the testis under local anesthesia, and using a syringe to aspirate small samples of testicular tissue containing sperm. The procedure can be performed as an outpatient procedure and typically takes less than an hour.
TESA can be an effective option for men with azoospermia who have failed to produce sperm with other methods such as testicular biopsy or microdissection testicular sperm extraction (micro-TESE). However, TESA is not always successful in retrieving sperm and may need to be combined with other techniques to increase the chances of success. It is important to discuss the benefits and risks of TESA with Genome consultant to determine if it is the most appropriate treatment option for each individual or couple.
Counselling:
Psychological counseling can be an important component of fertility treatment, as infertility can have a significant emotional impact on individuals and couples. Fertility treatment can be stressful, emotionally demanding, and can create feelings of anxiety, depression, and grief.
Psychological counseling can provide support and guidance to individuals and couples throughout the fertility treatment process. It can help them cope with the emotional and psychological challenges of infertility, address concerns related to treatment decisions, and help manage the impact of treatment on relationships and daily life.
Counseling can also help individuals and couples develop coping skills and strategies to deal with the stress of fertility treatment, such as relaxation techniques and mindfulness practices. It can also provide a safe and supportive space to discuss concerns related to fertility, sexuality, and relationships.
Counseling may also be particularly beneficial for individuals and couples who have experienced multiple failed fertility treatments or who are considering ending treatment. Counseling can provide support and guidance in making difficult decisions about the future of their family-building goals and help them manage the emotional impact of these decisions.
Overall, psychological counseling can be an important aspect of fertility treatment, providing individuals and couples with emotional support, coping strategies, and guidance as they navigate the challenges of infertility and treatment. We have trained psychological counsellor at genome to make the path to pregnancy as stress free as possible.